Team-Based Anesthesia Care: An Existing Idea Whose Time Is Now
/“Team-based anesthesia care” may sound like a brand-new concept, but the idea is actually rooted in over two decades of real-world practice here in Ontario, as well as influenced by other, similar models already in use in Canada and around the world.
Our section Vice-Chair, Dr. Sylvie Aucoin, knows that history. In addition to being an anesthesiologist at The Ottawa Hospital, she is a longtime advocate for team-based anesthesia care (TBAC). Below, she shares some of that history, as well as background on these innovative approaches to providing safe, accessible anesthesia care.
Q: What’s your connection to TBAC? Why are you interested in this topic?
A: I really became involved out of necessity. As the past Site Chief at The Ottawa Hospital (Civic Campus) and the Chair of the Canadian Anesthesiologists’ Society Hospital Chiefs of Anesthesia Section, I witnessed firsthand the detrimental impact of the anesthesiology human resource crisis on our patients, colleagues and the healthcare system locally and nationally. Across Canada, individual anesthesiology departments, hospitals, jurisdictions, organizations, and provinces are developing their own solutions in an attempt to maintain essential surgical services. It is critical to our patients and to our specialty that as physician anesthesiologists, we are leading and coordinating the development of these innovative anesthesia care models.
Learn more about TBAC and why the OA supports it.
Q: Before we had TBAC, we had Anesthesia Care Teams (ACTs). What are those and how are ACTs different from TBAC?
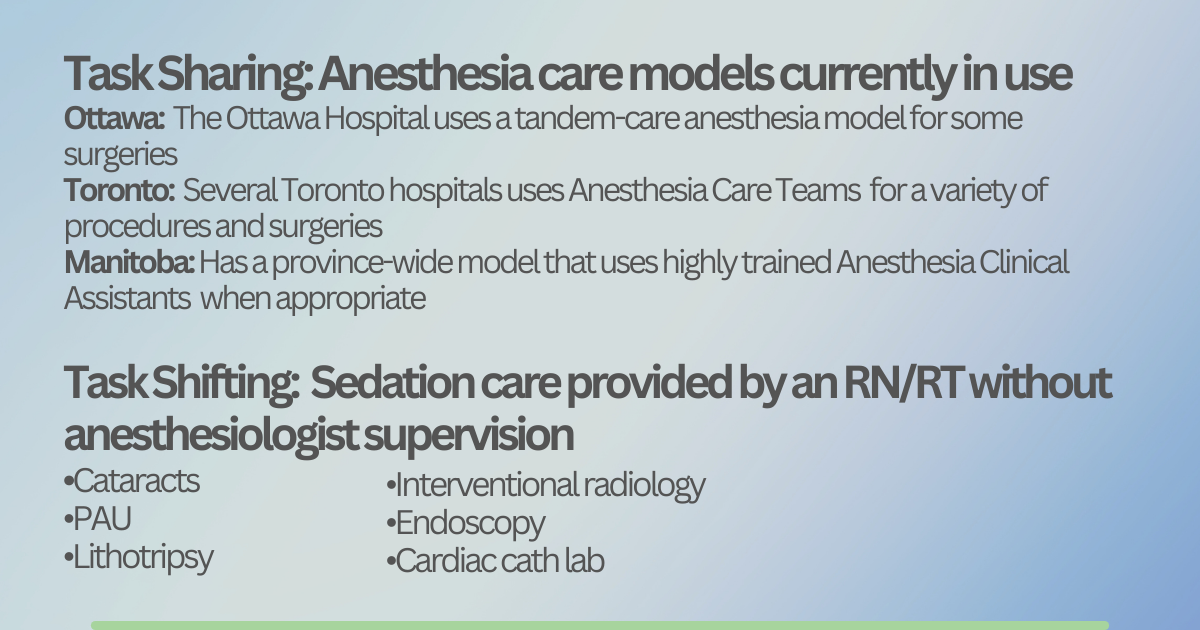
A: In Ontario, the anesthesia care team (ACT) model refers to the model developed over 20 years ago to improve access to cataract surgery. Light sedation for cataract surgery is provided by multiple anesthesia assistants or registered nurses being supervised by a physician anesthesiologist. Hospitals receive funding for the AAs and/or RNs working within this model and the anesthesiologists at a flat rate per case.
We are using the term “team-based anesthesia care” (or TBAC) to differentiate our current initiative from the ACT cataract model. TBAC covers more procedures than just cataracts and involves moderate and/or deep sedation or general anesthesia, but as with ACT, anesthesiologists continue to provide leadership, oversight, and critical decision-making for every patient under their care.
Q: We’re hoping to see an expansion of the TBAC model across the province. How would this rollout benefit patients?
A: The most obvious benefit is improved access to surgical care for our patients. A team-based care model will allow physician anesthesiologists to care for more patients by task-shifting less complex tasks to highly qualified physician extenders. Other potential benefits include improved patient safety; anesthesiologists often report risks to patient safety, moral distress, impact on provider wellness and reduced OR efficiency from inadequate anesthesia support. A thoughtfully designed anesthesia care team model would address many of these issues.
Q: Some hospitals in Ontario have been using TBAC for years. Can you share a few more details on that?
A: Unfortunately, since we rolled out the Anesthesia Care Teams to assist with increasing the number of cataract surgeries some 20 years ago, there has been no formal expansion of that or any other similar model. However, over the past few years, many hospitals, including my own in Ottawa and several in Toronto, have implemented their own “homegrown” version of TBAC to improve clinical care access. The OA is actively working to collect learnings from these centres to better inform how a province-wide TBAC model could look.
Existing task-sharing and task-shifting models that may inform how Ontario shapes team-based anesthesia care
Q: Versions of the TBAC model can be found around the world. What are some lessons that Ontario could learn from those other jurisdictions?
A: We don’t have to look very far: Manitoba implemented a TBAC model using anesthesia clinical assistants (ACAs) over 15 years ago. Their ACAs are registered with the College of Physicians and Surgeons of Manitoba as physician extenders and they have a well-thought-out entrustment scale.
We can learn from the models in the U.K. (anaesthesia associates) and the U.S. (certified anesthesiology assistants). Both are two-year Master’s training programs with strict admission requirements.
Q: What’s a key detail about TBAC that you wish people knew?
A: It’s important we recognize that TBAC is already happening in many centres across Ontario and nationally. Unfortunately, it has evolved without a provincial and/or national concerted and coordinated effort. The OA’s goal is to develop a provincial approach to physician-led TBAC that can be safely implemented in centres across Ontario. As the World Medical Association Resolution on Task Shifting recommends, physicians must be closely involved in all aspects of implementation, including training of this new cadre of assistants.
We also need to recognize that this is only one response to the anesthesia human resources crisis. We must continue to advocate for other solutions, such as increasing the number of anesthesiology and family practice anesthesia residency training positions, national physician licensure, and streamlining of processes for assessment and licensing of foreign-trained anesthesiologists.